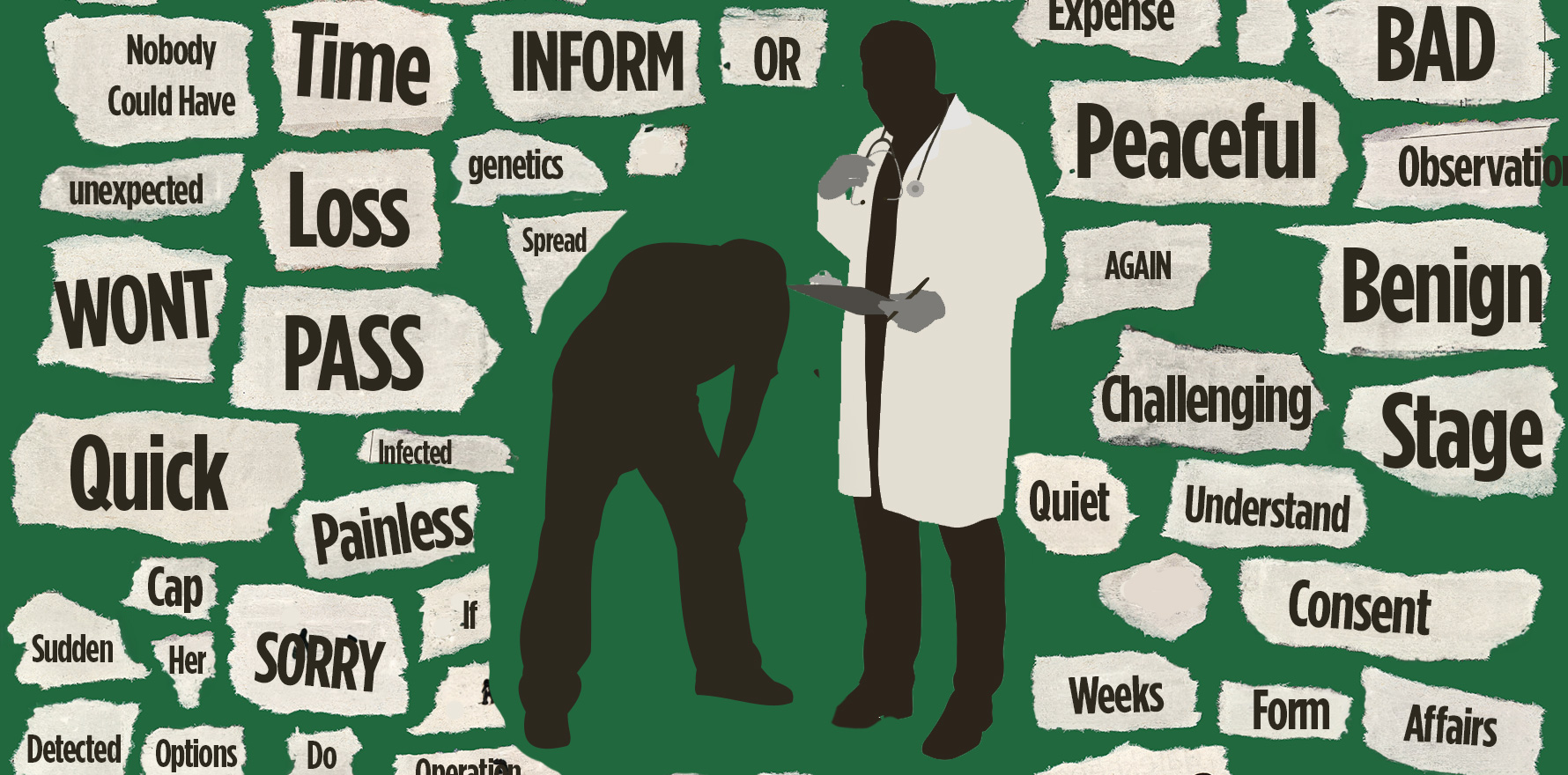
What happens when med school role-play ends and it’s just the GP and the patient in a quiet, sad, room?
In first-year medical school, we learnt how to break bad news. It was a clinical skills tutorial, and we role-played the doctor and the patient, alternating roles with our partner, waiting desperately for our turn to be the patient. Being the doctor, of course, is what we were training for but infinitely more nerve wracking and difficult. It was so much nicer and easier to be the patient. The one we could act as heartbroken, angry, disbelieving, comically dramatic and nonsensical.
We practiced breaking bad news again in second year in modern campus classrooms, then again in old decrepit tutorial rooms in the hospitals of third year, and again still in fourth year in the chaotic back offices of general practice surgeries. We role played scenario after scenario; confirmation of a suspected serious illness, a clinical error that resulted in a bad outcome, a clinical error that resulted in the worst outcome, a missed diagnosis, a very serious diagnosis detected incidentally. Every variation of breaking bad news was practiced, again and again, but not yet with a patient.
We tried the six-step SPIKES protocol of breaking bad news. We tried the five-step ABCDE. Someone taught us the BRAKES protocol. Someone else taught us SUNBURN. Guide after guide on how to deliver blow after blow. All the same in essence: prepare yourself and the patient, ensure privacy, be clear and direct, take time, take questions, clearly outline the next steps and follow up. Be compassionate albeit devastating.
As students, it felt awkward and unnatural, trying to role play these breaking bad news consultations, with our eyes constantly flickering to the framework written on the whiteboard, reminding ourselves to not miss a step. I remember once panicking at the end of a breaking bad news OSCE station because I had forgotten to provide the patient with a take-home brochure about their Bad Diagnosis (“So You Have Brain Cancer. What Now?”).
The truth is, like much of medical school, what we learn is completely different to what we practice. And how we practice what we learn is how we learn to practice.
In medical school, any bad news we break are just role-played. They’re pretend. They’re safe and protected and we have our training wheels on, riding tricycles on the kerb under the watchful eyes of doctors. Then we graduate and become interns and suddenly we’ve been upgraded to proper adult bicycles and told to ride in the bike lane on the road.
We’re asked by registrars to please let the patient in bed four know that she can’t go home yet because of her post-op ileus. Please let the family of the patient in bed 27 know that her kidneys are worsening and she may need dialysis. Please tell the patient in bed 18 that her emergency surgery has to be pushed another day because the consultant has to do a more urgent case. That the patient needs a PICC line. That he’s had positive blood cultures. That she needs an invasive biopsy.
The wards are terribly busy and the public hospital rooms have four beds in each. Patients are just separated by thin curtains, and the nurses want to get the discharges done ASAP. So, the bad news is often broken on ward rounds, in front of large intimidating medical teams at 7am with no family members there yet to support the sleep-deprived and sleepy-eyed patients. Curtains are pulled closed in a pathetic gesture of privacy, the blow is dealt, and then the team leaves to push through the hectic ward round and the intern is left to hurriedly pat the distraught patient for a moment – but only a moment – because she needs a good reference from the consultant leading rounds that morning and so she needs to move on and keep up.
As the junior doctor years pass, many of us pick up and cement these callous approaches to breaking bad news. SPIKES is forgotten and as distant a memory as the Kreb’s cycle and the brachial plexus. There is just too much sickness, the workload is crippling and we become increasingly desensitised. We just break bad news however we can in that moment and push through for ourselves and the patients. We deliver news unfeelingly, hastily, with no opportunity for privacy or questions and leave someone else to deal with the follow up. The oncology team perhaps, or the ICU Fellow. The nurse from palliative care.
I did it myself that way, innumerable times. Poor, unempathetic, half-hearted approaches to breaking bad news. It was very unfair. It was really quite heartless.
I only understood that when I became a GP registrar, and suddenly I was off the bicycle and put on a motorcycle speeding down the freeway. All the bad news I broke were to patients who were mine. People and families that I took ownership over, and responsibility. People who I expected to look after for decades, and perhaps the surviving ones I care for still. They were not strangers in a hospital bed, put there by the overnight registrar, waiting to be reviewed and emotionally destroyed by the new team in the morning and then returned to the care of some other.
In general practice, the patients came to me with the worrying symptom. It was my history, my examination, my detection of red flags that raised the concern. It was my name on the pathology form or radiology form, and it was me taking the urgent call from the radiologist reporting the abnormal findings. It was me asking the receptionist to urgently book the patient in the evening, at the end of an already long day, and it was me, the GP registrar, sitting down in a quiet room with the patient and their loved ones, breaking very bad news. It was me and my words alone that made it the worst day of that patient’s life. There was no consultant there, no team, no nurse. Just a quiet sad room, private and protected. Just the GP and the patient.
Breaking bad news isn’t like the med school role-plays at all, or the hospital years. It is much sadder, much heavier and often a great sense of hopelessness lingers. In almost fifteen years practicing medicine, it is the near-decade in general practice that made me expert at breaking bad news. I change the words I use or the approach I take for each patient. I intentionally choose the method or technique that I know will best suit this patient – a luxury I am afforded because as a GP, I know my patients pretty damn well. I schedule a hell of a lot of follow up, sometimes daily telephone calls to grieving relatives, and rarely do I send anyone home with a brochure. If they think of questions later, I welcome them back to ask me directly.
In general practice, when we break bad news, it is to people and families that we care for with fondness and intent. And after the patient is dead and gone, we will continue to care for the relatives that remain – motherless children, widowers or heartbroken sisters who grieve for the rest of their lives. They never forget that appointment, the one where we broke the bad news, and how it felt and how we did it. It’s often the opening line of the last chapter. The first sentence of the last paragraph. So, as GPs, let’s make sure we play the role really, mightily well, and hold our patients and ourselves with fragility and tenderness as we break bad news over and over and over again.
Dr Pallavi Prathivadi is a Melbourne GP, member of the Eastern Melbourne PHN Clinical and Practice Council, and GP Lead of the RACGP Academic Post cohort support and education program. She holds a PhD in safe opioid prescribing and was a Fulbright Scholar at the Stanford University School of Medicine. She is studying creative writing at Harvard University’s Division of Continuing Education.