Researchers propose that the antioxidative effects of magnesium may contribute to the findings.
The potential benefits of a magnesium-rich diet are more prominent in heavy drinkers compared to those who consumed less alcohol, researchers have found.
Magnesium deficiency is one of many factors that has been linked to the pathogenesis of cardiovascular disease and an increased risk of cardiovascular-related death.
Researchers believe that increased oxidative stress, a consequence of low magnesium levels, plays a role in the potential association between magnesium and CVD mortality. But no studies have specifically explored the link between a magnesium-rich diet and the CVD mortality.
That is, until now. A recent Chinese-led study, published in Atherosclerosis, used data from the US-run Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial to investigate the association.
Their findings suggest that high adherence to a magnesium-rich diet was associated with a substantially reduced risk of CVD mortality, for both heart and cerebrovascular disease.
“These findings support the magnesium-rich diet, characterised by higher consumption of wholegrains, nuts, fruits, vegetables, legumes, coffee and tea, as a beneficial dietary strategy for reducing CVD mortality,” they concluded.
Patients who completed the diet history questionnaire (a 124-item food frequency questionnaire that quantifies portion sizes, frequency of consumption and the types of foods and supplements consumed over the past year) at baseline with no history of cancer, stroke or heart attack were considered for the study.
A specific magnesium-rich diet score was calculated based on the responses to seven magnesium-rich foods – wholegrains, nuts, fruits, vegetables, legumes, coffee and tea – with higher scores representative of higher levels of magnesium in one’s diet.
Other behavioural and sociodemographic measures were captured at baseline. Annual follow-ups (to determine whether the patient was still alive) occurred via mailed questionnaires, family reports and death certificate checks.
A total of 91,891 individuals were included in the final cohort, with slightly more women than men (54% female). The average age of included participants was 65.3 years.
A greater proportion of people in the highest quartile for the composite magnesium-rich diet score reported higher levels of physical activity compared to individuals in the lowest quartile, while a smaller proportion smoked.
Participants in the highest quartile also had a lower BMI than participants in the lowest quartile. The median follow-up period was 15 years, with 5848 CVD deaths occurring during the follow-up. Roughly three quarters of CVD deaths (4236) were due to heart disease; the remaining proportion were due to cerebrovascular disease.
After adjusting for relevant confounding factors, patients in the highest quartile were 26% less likely to experience overall CVD mortality compared to patients in the lowest quartile (adjusted hazard ratio 0.74, 95% confidence interval 0.68-0.81). In addition, they were 26% less likely to experience heart disease mortality (aHR 0.74, 0.67-0.82) and 33% less likely to experience cerebrovascular disease mortality (aHR 0.67, 95% CI 0.56-0.81).
Further analyses revealed a dose-response relationship between the magnesium-rich diet score and CVD mortality, where higher scores were associated with a lower hood of dying.
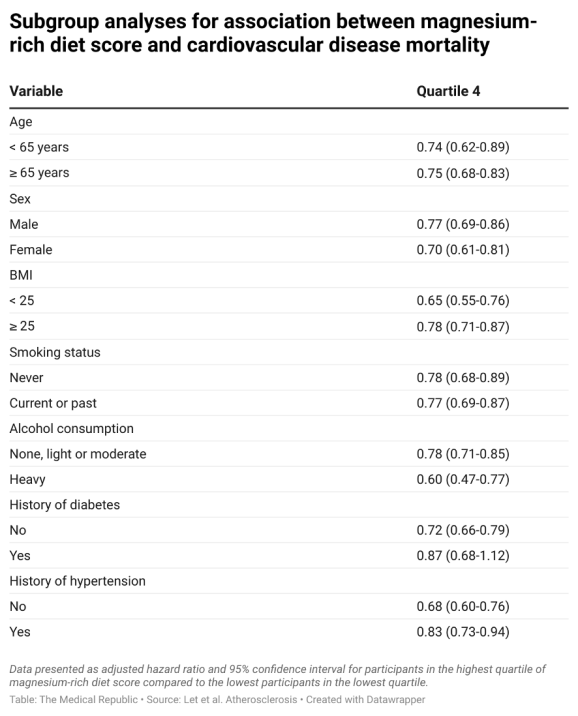
Pre-planned subgroup analyses showed the observed association between the magnesium-rich diet score and CVD mortality in most of the examined cohorts, although the authors did observe a stronger negative association between the exposure and outcome in heavy alcohol drinkers compared to non-, light- or moderate drinkers.
The researchers suggested numerous mechanisms that could explain their reported association between a magnesium-rich diet and lower CVD mortality.
“Magnesium exerts antiarrhythmic effects by modulating intracellular ion transport systems for sodium, calcium and potassium, reducing early after-depolarisations, and slowing atrioventricular nodal conduction. These effects may lower the risk of sudden cardiac death,” they wrote.
“Second… oxidative stress is a major contributor to CVD progression, as excessive reactive oxygen species production overwhelms antioxidant defences… Magnesium-rich foods supply antioxidant constituents, including magnesium itself, dietary fibre and vitamin E, which may collectively counteract oxidative status.
“Third, a magnesium-rich diet provides synergistic actions of multiple nutrients and bioactive compounds, including minerals, vitamins and polyphenols, which may exert lipid-lowering and anti-atherogenic effects. These include inhibition of low-density lipoprotein oxidation, modulation of lipid metabolism and improved endothelial function.”
Potential explanations for the stronger effect of magnesium-rich diets in heavy drinkers compared to people with low- or no alcohol intake were also discussed.
“Chronic alcohol use increases urinary magnesium extraction and depletes body magnesium stores, resulting in hypomagnesemia. Magnesium deficiency in alcoholics may enhance platelet hyperaggregability, accelerating atherosclerosis and elevating hypertension risk,” they wrote.
“High concentrations of ethanol reduce coronary blood flow, deplete cellular magnesium, promote myocardial metabolic acidosis, cause sarcolemmal damage and lead to calcium overload.
“These combined mechanisms predispose individuals to acute cardiac events and heart failure.”
The researchers also suggested there was evidence that magnesium supplementation can reverse these alcohol-induced changes.
They noted the significant findings must be interpreted with caution, as the study design did not allow them to determine a causal link between magnesium-rich diets and cardiovascular mortality risk.
In addition, any association between diet and cardiovascular outcomes was limited to considering magnesium intake was assessed through an indirect dietary questionnaire, rather than measuring isolated magnesium intake – meaning the effects of other individual nutrients and bioactive compounds could not be controlled for.


